Infertility is usually defined as the inability to conceive despite regular sexual intercourse for more than 12 months. This article will address primarily female infertility or “female-factor” infertility.
In the conventional Western medical paradigm, a woman’s advanced age, hormonal abnormalities, tubal-, uterine-, or endometrial-related conditions are common causes of female infertility. In men, infertility is seen to occur due to poor sperm quantity and/or quality and spermatogenesis as well as erectile dysfunction.
In both sexes, psychosomatic aspects and stress levels are important but rarely addressed. Ayurveda would add another unique aspect as well which impacts fertility–karmic effects. Frequently we see infertile couples in whom standard investigations including hormonal levels, semen analysis, ovulation testing, and tubal patency are normal. This accounts for 25-30% of all couples seeking help.
The complete evaluation for female infertility includes patient history, gynecological examination, record of basal temperature, vaginal and cervical cultures, ultrasound studies, hormonal analysis [i.e. follicle stimulating hormone (FSH), luteinizing hormone (LH), prolactin, testosterone, dehydroepiandrosterone sulfate (DHEAS), and thyroid-stimulating hormone (TSH)], hysterosalpingogram with dye to visualize the fallopian tubes, and semen analysis of the partner.
Depending on the presumed cause(s) of female infertility conventional drug treatment can include any of the following:
- Gonadotropins in the case of hypogonadotropic ovarian failure
- Selective Estrogen Receptor Modifiers (SERMs) like clomiphene
- Prolactin inhibitors in the case of hyperprolactinemia
- Metformin in the case Polycystic Ovarian Syndrome (PCOS)
- Progestogens, surgical measures to lyse adhesions in case of endometriosis
- Gonadotropin Releasing Hormone (GnRH) in case of hypothalamic ovarian failure
However, the most common treatment offered for most women is in vitro fertilization (IVF) with or without intracytoplasmic sperm injection (ICSI).
In Vitro Fertilization is a very recent and still evolving treatment. The first pregnancy using it was in 1973, however it ended after a short time in a miscarriage. Back then it was making a great deal of news and controversy and the phrase “test-tube baby” was in the headlines. A second pregnancy was recorded in 1976, however, the embryo was embedded in the fallopian tubes and had to be surgically removed. In 1977, a study with 68 women was conducted, resulting in only two pregnancies: one woman having a deformed, still-born child, and another woman requiring an abortion. Altogether, up to the birth of the first successful IVF child, only about 200 embryos transfers were attempted.
In 1978, the first child was born using IVF in England (Louise Brown, age 38 today). In the U.S. it happened in 1981. I recall at that time the news was met with both amazement by some and revulsion by others.
Today the procedure has changed greatly from those early days, but it’s certainly not a simple or natural process. First, a medication is given to suppress the woman’s LH surge and her ovulation until the developing eggs are ready. This drug is commonly a GnRH-agonist (gonadotropin releasing hormone agonist) such as Lupron. Next an FSH analog (follicle stimulating hormone) is given to stimulate (hyperstimulate, in my opinion) development of multiple eggs (Gonal-F and Follistim are the most common).
Finally HCG (human chorionic gonadotropin) in a usual dose of 10,000 mIU/mL is given to cause final maturation and ovulation of the eggs. The eggs (oocytes) are collected and assessed for their health and degree of maturity. Following preparation of the ejaculate, insemination takes place by mixing the eggs and sperms. A maximum of 3 embryos are transferred to the uterus. The embryo, at this point, is in the four- to eight-cell stage.
In addition to IVF, ICSI has also been introduced in cases of more complex male subfertility (insufficient sperm count or motility). In this procedure a single spermatozoon is injected directly into the cytoplasm of the oocyte using a micropipette.
After 48-72 hours the embryo is transferred into the uterus. After transferring the embryo, implantation is no longer controllable, and everyone waits and hopes. The ensuing 2-week luteal phase is supported with medication (commonly progesterone injections every day!). Using IVF with intra-cytoplasmatic sperm injection and subsequent embryo transfer, most Reproductive Medicine centers around the world claim their rate of successful pregnancy is around 60%; the “baby take home” rate depends on the age of the mother ranging from about 40% for women under 35 to about 10% if over 40.
The physiology of the reproductive system as a whole is governed by sadhaka pitta, prana vata, and apana vata, yet the reproductive organs themselves are endowed with the qualities of kapha. Kapha is the growth-promoting (anabolic), structure-forming dosha that generates and sustains creation. Together with ojas (life force) and rasa dhatu (plasma tissue), kapha dosha organizes the nourishment required to build and re-build the endometrial lining during a lifetime of artava (menstruation) and has an unctuous quality that lubricates the uterus and its ‘sister’ organs (e.g. ovaries, fallopian tubes, cervix, vaginal canal). Kapha also confers stability and strength to the reproductive tissues helping maintain ovarian structure and uterine shape, tone and ability to contract.
A woman whose artava is exhausted, is called vandhyatva (vandhya-barren, childless). This disease entity—vandhyatva—is the condition closest to infertility in the Ᾱyurvedic classification of diseases. Detailed diagnostic and therapeutic strategies were already described as early as 200 AD in the authoritative Ᾱyurvedic text Caraka Samhita (chapter Cikitsa-sthana, Yonivyapat).
In the centuries that followed, specialized texts on gynecology evolved, including the Kashyapa-Samhita which contains detailed descriptions of various diseases and dedicates a complete chapter to female infertility. As we shall see below, both samshamana (gentle) and samshodhana (strong) therapies are advised for the treatment of infertility in Ᾱyurveda.
The main Ᾱyurvedic treatment goals are (1) the purification and (2) the functional optimization of reproductive tissues (artava- and shukra-dhatu) of both sexes. According to Ᾱyurveda, reproductive health is primarily determined by the health of tissue metabolism and tissue nutrition, both being ultimate requirements for conception. The presence of any accumulated tissue toxins will hamper treatment.
Therefore, general panchakarma purification measures must almost always be the initial step in the treatment sequence. Depending on the Prakriti (unique constitution) of the individual these purification measures may include emesis, purgation, medicated enema, blood purification, and several other specific procedures pertinent to reproductive health. One such example is uttara-basti, intrauterine douche with medicated oils or decoctions. A description of the complete range of these specialized treatment options is beyond the scope of this article.
As Ᾱyurveda is a holistic science, it is important to always consider the patient’s overall health condition, including her mental health and living environment. Importantly, the unique feature of the Ᾱyurvedic approach to fertility is that it emphasizes improving the overall health of both the prospective parents. Fertility therefore may ensue partly due to improved overall health. This approach contrasts with the biomedical approach, which does not directly consider overall health and narrowly focuses on the reproductive tissues.
After thorough patient history taking (prashna) including modern and Ᾱyurvedic parameters, the eightfold and tenfold diagnostic processes (ashtasthana– and dasha vidha-pariksha) are performed according to traditional diagnostic principles of Ᾱyurveda (see below). Patients are understood by Ᾱyurvedic diagnosis as having a particular sub-type of vandhyatva based on their doshic constitution (prakriti).
The most obvious and relevant pathological findings in all cases of infertility from the Ᾱyurvedic perspective are: (1) an overall imbalance of all of the 3 doshas (sannipata-prakopa of vata-, pitta- and kapha-dosha), but usually with dominating kinetic and metabolic principles (vata and pitta) and (2) an irregular functioning of the digestive principle (agni) at both the organ and cellular levels, (3) srotodushti, obstruction or blockage of the channels for both gross and subtle nutrients and energies.
According to the Ᾱyurvedic explanatory model for etiopathogenesis/disease staging (samprapti), most woman, by the time they are aware of any problem, are in the fifth stage of the disease sequence (manifestation or vyakti) or the sixth and latest stage (chronic disease or bheda).
Ashtasthana Pareeksha (Eightfold Examination)
Nadi – Pulse diagnosis
Mutram – Urine examination
Malam – Fecal matter examination
Jihwa – Tongue and taste assesment
Sabdam – Voice and speech of the patient; heart, lung and abdominal sounds
Sparsham – Touch, skin and tactile sense
Driksha – Eyes and vision
Akriti – General physique (i.e. lean, muscular, etc.); general complexion
Dasavidha Pareeksha (Tenfold Examination)
Dushyam- Regarding the structural and functional abnormalities of the body
Desham -Geographical situation of the place where patient lives (eg: marshy)
Balam -Physical strength
Kalam- The season and climatic conditions
Analam -The digestive system of the patient
Prakriti- The natural Tridosha constitution of the body
Vayas -Age of the patient.
Satvam- Psychological strength of the patient
Satmyam- General and personal habits of the patient e.g. tobacco use, regular exercise, yoga asana practice, napping, etc.
Aharam- Nature of food (e.g. vegetarian or non-vegetarian)
Although there are usually strategies to neutralize the negative effects of most conditions, one should be aware of the influence of all aspects of health on female fertility. Here I will mention a few of the more common ones. Chronic menstrual irregularities and associated symptoms like excessive bleeding and severe cramping represent signs of imbalanced gynecological functions (apana vata prakopa and artava dhatu-dushti); anatomical abnormalities (ovarian cysts, retroverted or T-shaped uterus, etc.) also have significance (vata-kapha prakopa). Previous Caesarian section, curettages, miscarriages, intramural pregnancy with iatrogenic abortion, and IVF procedures represent traumas to the reproductive tissues (vata, particularly apana-vata, rakta dhatu-dushti, etc.), leaving scars and leading to a ‘channel obstruction’ (sroto-rodha) of apana-vata, the subdosha regulating gynecological functions; ovarian cysts (artava-dhatu-vrddhi and vata-kapha-prakopa) interfere with implantation. The ovarian hyperstimulation with FSH drugs which is casually recommended by doctors certainly causes significant Vata aggravation (vata-prakopa).
Lyme disease, multiple sclerosis, Hashimoto thyroiditis, allergies, obesity, anorexia, irritable bowel syndrome as well as any other low-grade chronic inflammatory condition are indicators of a generally disturbed immune system (rasa-kshaya, rakta- and majja-visha and ojovyapat (loss of vitality) with vata as dominant active factor) – creating a suboptimal environment for implantation and conception in general. Any history of drug intake or environmental exposures is another inhibiting factor for natural fertilization according to Ᾱyurveda, which is why Panchakarma is so vitally important. Sleeping disorders engender mental stress weakening both physical and emotional stability. Furthermore, there can be any number of other factors which create imbalances (e.g., excessive traveling, job stress, relationships, moving to a new home, illnesses in the immediate family, etc.).
Except for acute causes such as the various traumas listed above, female infertility is almost always a result of a gradually-incremental, slowly developing disease process. The holistic Ᾱyurvedic treatment to any disease or condition, including infertility, utilizes a multimodal approach. Both samshodhana (strong; purifying) and samshamana (gentle; balancing) treatments are always used.
Ᾱyurvedic treatments are not merely a series of single and autonomous treatments, but on the contrary, are a carefully formulated highly-individualized and complex arrangement of treatments whose functioning can only be understood if viewed as an integrated whole. A defining feature of the holistic-oriented Ᾱyurvedic strategy is the therapeutic integration of the physical (e.g. purification through Panchakarma, dietary recommendations, herbal medicines, etc), psychological, and spiritual realms (e.g. mantra recitation, use of gemstones, placement of sacred objects in the home, prayer, etc). In Ayurveda, female infertility is understood as a somato-psycho-spiritual disintegration with a tendency to somatize unresolved emotional and mental conflicts; these conflicts are either wholly or partially causative or they further aggravate co-existing epigenetic, traumatic, and biochemical causes.
The selected purification methods (most commonly purgation, enemas, intrauterine enemas and nasal irrigation) are delivered to restore balance to the kinetic vata principle, according to Ᾱyurvedic theory. The far-reaching therapeutic benefits for this are difficult to explain through conventional modern pathophysiological principles. A detailed explanation of Ayurvedic theory and energetics though fascinating and compelling is beyond the scope of this article.
However, what can pragmatically be said here is that these methods optimize mucosal transport and general function, regulate and stabilize the intestinal microbiome, restore hormonal homeostasis to the interior milieu, enhance intestinal digestion, metabolism and excretion, and counteract side effects of both endogenously-produced and environmental toxins. These effects are augmented if the individual is concurrently observing an appropriate individual dietary approach, receives the appropriate herbal medicines, and also follows the other prescribed Ᾱyurvedic principles.
Here is a brief description of some of the Ᾱyurvedic approaches used and the reasoning behind them. Not every therapy is used for every woman and they are always modified according to the individual constitution.
Virechana (purgation): This procedure involves several days of internal oleation by taking either pure ghee or a specially prepared medicated ghee followed by a gentle herbal purgative. Purgation acts on aggravated and accumulated pitta and kapha doshas. It decreases the heat (ushna guna) of pitta and increases coolness (sheeta guna) required for formation of shukra dhatu (ovum and sperm). Impaired agni due to disturbed pitta is also rectified by the virechana procedure. A strong and balanced dhatvagni (tissue agni) is required for dhatnirmiti of shukradhatu (creation of reproductive tissue). Obstructing kapha dosha is removed through virechana and the blocked apana vata obstructed by kapha dosha is also relieved by virechana. Common virechana dravyas: mahatiktaghrit, trivrit (leha or churna).
Anuvasana and Niruha Bastis (medicated enemata): These are two different types of medicated enemas. The reproductive system present in katisthana (hip and loin region) which is a region chiefly regulated by of apana vata. Action of basti is predominantly on vata dosha and pakvashaya (large intestines). The uterus (garbhashaya) is made up of vayu and akasha mahabhuta. In basti, mainly tiktarasadravya (vayu + akasha mahabhutas) despite being potentially vatavardhak (vata-increasing), are useful because they act as a vehicle and catalyst to deliver medicines to vatasthana (vata regions). Sneha in basti promotes trans-membrane absorption of herbal medicinal components. Since Basti is targeted at regulating the apana vata, it facilitates the well-timed release of ovum and also normal motion of sperms.
Uttar Basti (medicated intrauterine enema): Uttar basti plays a very prominent role in treating female infertility because it has a direct local action upon the reproductive tissues. The ovaries contain receptors which receive hormones secreted by the hypothalamus and pituitary gland. The herbal medicines used in uttar basti stimulate and sensitize these receptors, so that proper ovulation occurs in each cycle. It also helps to increase the receptivity of the genital tract to the entry of sperms.
In addition, uttar basti relieves artava srotosanga (congested channels of menstrual flow) and corrects artava dhatvagni (reproductive metabolism). Because selected medicines are administered directly to affected areas, it can help clear tubal blockage by direct lysis of adhesions. Finally, altered cervical pH can be corrected by uttar basti. Depending on the specific issue identified, different uttar basti dravyas are used. For example: in ovulatory disorders: shatavarighrita, balaguduchyadi taila, phalaghrita; in tubal obstruction: kshar taila, bhallataka taila, til taila; in uterine fibroids or PCOD: dashmoola taila, panchatiktaguggulghrita, varunadi kwath, hapushadi ghrita.
Nasya (administration of nasal medications): All Ᾱyurvedic students learn the sloka: “nasya hi shiraso dwaram,” which means “the nostrils are the gateway to the brain.” Therefore any substance introduced intranasally (even smoke) acts directly on the brain and specifically in this context, the hypothalamus and pituitary glands.
Today we know that the olfactory nerve fibers literally enter the back of the nasal passage through the cribiform plate and conveys stimuli directly to the brain. The mucosal epithelium is sensitive to a variety of stimuli including various herbalized ghritas and tailas which are easily absorbed through mucosal epithelium. Nasya medications may help to stimulate the hypothalmal- pituitary axis to secrete FSH & LH hormones. We often use chandanbala taila, shatpushpa taila, and phalaghrita.
Adjuvant Panchakarma Treatments: The specialized physical therapy techniques, including Shirodhara (forehead-dripping therapy), Shirobasti (oil-crown), and Lepa (herbalized mud) with precisely selected medicated oils and other substances, further facilitate the stabilization of the overall constitution by balancing the impaired vata and pitta doshas.
Oral Herbal Medicines: While it is beyond the scope of this article to describe the many individualized formulas which can be used as part of the treatment for vandhyatva, it can be stated that Ᾱyurvedic herbal formulas used in these patients primarily target adaptogenic, rejuvenative, aphrodisiac, and general strengthening (ojo vardhana) as well as strengthening of the reproductive tissues; they also are designed to enhance digestion and cognition as needed and have mild anxiolytic and antidepressant properties.
That being said, some of the more common plants used include Ashwagandha (W. somnifera), Shatavari, (A. racemosus), Guduchi (T.cordifolia), Brahmi (B. monnieri), Yogaraj guggulu, Krishna Jeeraka (N. sativa), Shatapushpa (A. graveolens), Atibala (A. indicum), dashmoolarishta, maharasnadi kwath.
Lifestyle Factors: In a similar way to everything mentioned above, yoga, meditation, and mantra recitation address the physical and mental stress caused by the often numerous futile fertility attempts with conventional therapy. One other interesting practice is to have a woman simply place a stone shiva linga of any size under the foot of her bed. The connection between detoxification, stress and infertility is not yet well understood. However, in my more than three decades of Ᾱyurvedic practice, it is not uncommon to see patients finally give up IVF, undergo Panchakarma and Ᾱyurvedic protocols–and then become pregnant shortly thereafter. Once the stress, expectations, and adverse physiological effects of IVF treatment subside, the body is sometimes able to function normally again. That is why from the Ᾱyurvedic perspective, these seemingly gentle mind-body recommendations are effective; they also target the regulation of vata, in this case on the level of manas (i.e. the mind).
Despite the many successful case reports in India and other Ayurvedic clinics around the world, it remains an open scientific question whether the Ᾱyurvedic approach exerts any specific fertility-promoting effects. Besides my own U.S.-based medical practice, the effectiveness of Ᾱyurvedic interventions is based primarily on numerous case studies and rather small and mostly preliminary clinical trials conducted in India. From the perspective of modern scientific research, given the many successes documented and despite the lack of well-designed randomized controlled studies, further research is warranted. In particular, the integration of Ᾱyurvedic treatments into modern medical strategies for fertility has the potential to improve patient outcomes with little to no downside.
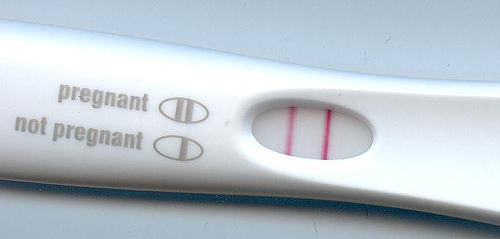
Image: Unsplash.com
Click for detailed story

 When you consider all the changes in our agricultural practices, the increased number of medications we take, as well as our dependence on plastic and technology that is constantly emitting low-grade radiation, it’s no surprise more couples are having trouble conceiving. Current statistics show one in six couples who are trying to conceive are facing fertility issues. And while many times infertility is thought of as a female issue, it is really a factor for both the man and woman and should therefore be addressed as such.
When you consider all the changes in our agricultural practices, the increased number of medications we take, as well as our dependence on plastic and technology that is constantly emitting low-grade radiation, it’s no surprise more couples are having trouble conceiving. Current statistics show one in six couples who are trying to conceive are facing fertility issues. And while many times infertility is thought of as a female issue, it is really a factor for both the man and woman and should therefore be addressed as such.